Spinal fusion surgery has been used to improve the quality of life for hundreds of thousands of people worldwide. Effective for treating a variety of back and spine-related conditions, it’s a common surgical measure for dealing with spinal degeneration or pain-related issues.
Spinal Fusion
Is spinal fusion surgery right for you?
Spinal fusion is a surgical procedure used to link together — or fuse — two or more vertebrae in the back, so there is no movement between them.
Spinal fusion is frequently required after an injury, infection, or tumor to stabilize the spine and alleviate pain. It’s a procedure that can help restore stability, reduce pain-related issues and restore quality of life.
This type of surgery can be particularly useful for degenerative conditions such as spondylolisthesis1. However, spinal fusion is not typically recommended in instances where the cause of the pain is non-specific or unidentified, for example, in lower back pain without a clear cause2.
Common spinal fusion procedures performed at Texas Health Center for Diagnostics & Surgery include:
Neck
Cervical (neck) fusion
Cervical fusion is a surgical procedure that links together damaged segments of the vertebral column in the neck. Cervical spinal fusion surgery is most frequently used to stabilize the spine. However, it is most often performed for degenerative conditions, to take the pressure off the nerves in your neck and stabilize the spine, helping relieve pain in the process.
Anterior cervical fusion
The anterior approach to cervical fusion — also known as an ACDF (anterior cervical discectomy and fusion) — entails surgeons operating through the front of the neck as opposed to the back of the neck. Carried out under general anesthesia, the relevant muscles and blood vessels are temporarily moved aside so that the surgeon can access the spine itself.
Posterior cervical fusion
Posterior cervical fusion is performed through an incision in the back of the neck. Both anterior and posterior access have their own particular uses, and your surgeon will advise which is preferable for your condition before carrying out the procedure.
Lower Back
 Lumbar fusion is one of the most common surgical approaches for treating lower back pain. And there are a wide number of techniques used to perform a lumbar fusion, all with the goal of fusing the vertebrae together. Each procedure has its own advantages and disadvantages that your surgeon will discuss with you. Some of these techniques include:
Lumbar fusion is one of the most common surgical approaches for treating lower back pain. And there are a wide number of techniques used to perform a lumbar fusion, all with the goal of fusing the vertebrae together. Each procedure has its own advantages and disadvantages that your surgeon will discuss with you. Some of these techniques include:
Posterior lumbar fusion
Posterior lumbar fusion is the most common type of fusion surgery for low back pain. It is used to treat spine instability, severe degenerative disc disease, and fractures in the lumbar spine. With this surgery, two or more vertebrae are fused together into one solid bone. During the procedure the spine is accessed through an incision in the back. It may be performed by traditional open spine surgery or by minimally invasive methods, depending on which approach best addresses the patient’s needs and anatomy. Instrumentation such as screws and rods will be used to stabilize the spine.
Lateral interbody fusion surgery
This type of minimally invasive surgery is performed by approaching the spine from the patient’s side to remove the disc tissue causing pain and to join two or more vertebrae together.
Anterior lumbar interbody fusion (ALIF)
Anterior lumbar interbody fusion is performed by approaching through the patient’s abdomen. a type of spinal fusion used for treating problems such as disc degeneration, spine instability, and deformities in the low back area of the spine. An incision is made in the abdomen, the disc material is removed, and the lumbar spine bones are fused together.
Transforaminal lumbar interbody fusion (TLIF)
Transforaminal lumbar interbody fusion is a surgery in which the front part of the lumbar spine is fused from the back. that involves the removal of a disc between two vertebrae and fusing them together. This type of surgery is recommended for those suffering from degenerative disc disease and other conditions that cause low back pain. This surgery is performed approaching the spine from the back.
Anterior/Posterior lumbar fusion (360)
This procedure involves fusing the spine from both the back and the front. It’s quite common for lumbar fusions, as it involves an entry through both the abdomen and the back — this allows the surgeon to work more easily on the spine.
New Technologies for Spinal Fusions
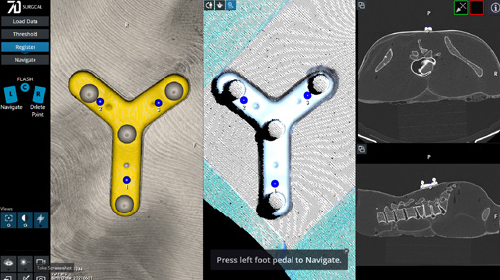
The 7D FLASH™ Navigation System employs advanced MvIGS (Motion vision Image Guided Surgery) technology to offer radiation-free guidance during spinal procedures. Think of it as a GPS for your surgical team, creating a 3D image of the patient's spine using visible light and machine-vision algorithms. This enables surgeons to operate with enhanced precision and efficiency.
Unlike traditional methods, it eliminates intraoperative radiation, reducing exposure for patients and health care providers. Highly detailed guidance and real-time navigation not only help surgeons navigate complex spinal anatomy with greater precision, reducing the risk of complications, but it also streamlines surgeries, potentially leading to shorter operating times.

Same Vision, New Views
Powered by the same 7D Technology listed above, the FLASH™ Percutaneous platform does not require an open surgical site, making it ideal for minimally invasive spinal procedures. Utilizing special cameras and visible light, the system quickly looks at the unique shape of the patient's spine and anatomy. This then creates a full-color 3D image reconstruction consisting of almost one million data points used for surgical navigation, thus providing the same fast, accurate and efficient surgical workflow.
Understanding the risks
Spinal fusion can be carried out very safely. However, like any other major surgery, it does carry certain risks and the potential for side effects. Some of the most common risks can include:
Reduced mobility
Although spinal fusion surgery can be very effective at restoring quality of life and reducing pain, it can sometimes be at the cost of slightly more restricted movement. There may be certain activities that you’re no longer able to participate in, such as contact sports. Although for most patients, this is a trade-off that they’re willing to make, it’s still something worth considering prior to surgery.
Potential future surgeries
Fusion can be a very effective way to address pain and other issues, but it may be necessary to have future fusions over time. This can occur due to other nearby vertebrae absorbing additional stress and deteriorating more quickly.
However, your surgeon will discuss all of these risks prior to performing the surgery. You will be able to make an informed decision about whether this is the right option for your particular spine issues.
Disc replacement as an alternative to spinal fusion surgery
In certain instances, it may be possible to opt for disc replacement surgery rather than spinal fusion surgery. In cases where a lumbar or cervical disc has been damaged, herniated, or has simply deteriorated, disc replacement may be another option.
Disc replacement is typically less invasive than spinal fusion and has a quicker recovery time. It also tends to avoid some of the side effects associated with spinal fusion, such as adjacent level deterioration. However, it’s not suitable in every instance — if the bone itself is the issue, then spinal fusion may still be the most appropriate option.
If you are interested in finding out if disc replacement surgery is right for you, get in touch with the Center for Disc Replacement today!
[1] https://journals.lww.com/neurosurgery/pages/default.aspx
[2] https://pmc.ncbi.nlm.nih.gov/articles/PMC5333707/
Contact us for more information
If you have additional questions about our spine services or would like more information about treatment options, please call our patient navigator at 972-543-1250 or